Symptoms of Nipah Virus Infection: A Complete Guide (2026 Update)
Symptoms of Nipah Virus Infection: A Complete Guide (2026 Update)
Author: Health & Wellness Editorial Team
Date: January 26, 2026
Target Audience: India & South East Asia
Introduction: Why You Need to Know the Symptoms in 2026
As we navigate through January 2026, the resurgence of the Nipah virus in parts of India, specifically the recent alerts in West Bengal (Barasat and Kolkata regions) and the lingering vigilance in Kerala, has brought this deadly pathogen back into the spotlight. Unlike the common flu or seasonal viruses, Nipah is a high-consequence pathogen with a fatality rate that can range from 40% to 75%.
Understanding the symptoms of Nipah virus infection is not just about awareness—it is a critical survival skill. Early detection can mean the difference between life and death, not just for the patient but for their caregivers and family members. This comprehensive guide will walk you through everything you need to know about the signs, risks, and the latest medical updates available in India as of 2026.
What is Nipah Virus?
The Nipah virus (NiV) is a zoonotic virus, meaning it spreads from animals to humans. In India, the primary carriers are fruit bats (flying foxes). However, the virus is not limited to bats; it can infect pigs and, most alarmingly, can spread directly from human to human.
While outbreaks are sporadic, the 2026 clusters have reminded us that the virus is always lurking in the natural reservoir. The World Health Organization (WHO) has listed Nipah as a priority disease requiring urgent research and development.
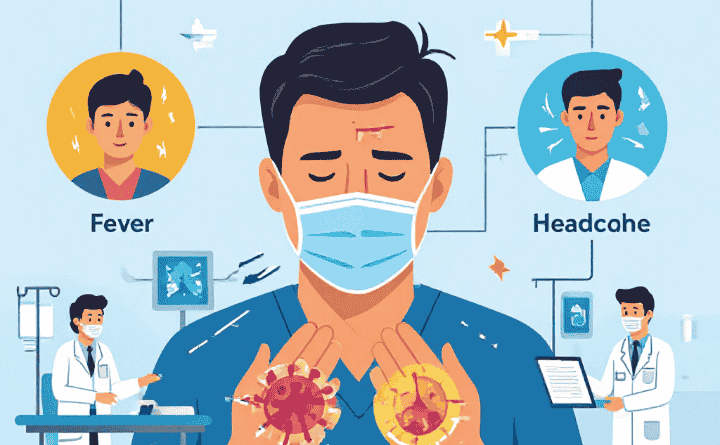
Detailed Symptoms of Nipah Virus Infection
The clinical presentation of Nipah can vary widely. Some people may remain asymptomatic (showing no symptoms), while others develop acute respiratory distress and fatal encephalitis (brain inflammation).
1. The Incubation Period
Before symptoms appear, there is an incubation period.
- Standard duration: Typically 4 to 14 days after exposure.
- Extended duration: In rare instances, the incubation period has been reported to be as long as 45 days.
- Implication: You might feel perfectly healthy for two weeks after exposure while still potentially harboring the virus.
2. Early Symptoms (The “Flu-Like” Phase)
The infection often starts innocuously, mimicking a standard viral fever. This is why it is often misdiagnosed initially. If you live in or have visited a high-risk area (like containment zones in Kerala or West Bengal), watch out for:
- High Fever: Sudden onset of high temperature.
- Headaches: Severe, throbbing headaches are a hallmark sign.
- Myalgia (Muscle Pain): Intense body aches and weakness.
- Sore Throat: Irritation and pain in the throat.
- Vomiting: Nausea and recurrent vomiting.
- Respiratory Issues: Cough and difficulty breathing are common, especially in the Bangladesh/India strain of the virus.
Critical Note: If you experience these symptoms after consuming raw date palm sap or being in contact with a known patient, seek immediate medical isolation.
For more detailed global data, you can visit the <a href=”https://www.who.int/health-topics/nipah-virus-infection” target=”_blank”>World Health Organization (WHO) Nipah Overview</a>.
3. Progression to Severe Symptoms
The virus can progress rapidly. In many cases, the transition from mild symptoms to a critical state happens within 24 to 48 hours. The virus targets the central nervous system, resulting in:
- Dizziness and Drowsiness: The patient may feel constantly sleepy or unable to stay awake.
- Altered Consciousness: Confusion, disorientation, and inability to recognize family members.
- Acute Encephalitis: This is the swelling of the brain, causing severe neurological distress.
- Seizures: Uncontrollable convulsions are common in severe cases.
- Coma: Without rapid supportive care, the patient may slip into a deep coma.
- Acute Respiratory Distress: Severe pneumonia-like symptoms where the lungs fail to provide enough oxygen.
4. Long-Term Effects (Post-Recovery)
Survivors of the Nipah virus face a tough road ahead. Even after recovery, around 20% of patients are left with residual neurological conditions, such as:
- Persistent seizure disorders.
- Personality changes.
- Relapsed Encephalitis: In rare cases, the virus can become dormant and reactivate months or even years later, causing death.
How Does Nipah Spread? (Transmission)
To prevent the symptoms of Nipah virus infection, you must understand how it enters the human body.
- Bat-to-Human: The most common route in India and Bangladesh is the consumption of raw date palm sap (Toddy) or fruits that have been bitten by infected fruit bats.
- Animal-to-Human: Contact with infected pigs or other domestic animals (though less common in the Indian context compared to Malaysia).
- Human-to-Human: This is the biggest risk during an outbreak. The virus spreads through body fluids (saliva, urine, blood, respiratory droplets). Caregivers and healthcare workers without proper PPE are at the highest risk.
Diagnosis and Treatment: The 2026 Landscape
Diagnosis
Doctors use a combination of tests to confirm the virus:
- RT-PCR (Real-Time Polymerase Chain Reaction): Performed on throat swabs, nasal swabs, urine, or cerebrospinal fluid during the acute phase.
- ELISA (Enzyme-Linked Immunosorbent Assay): Used to detect antibodies later in the infection or after recovery.
Treatment Status in 2026
As of January 2026, there is still no globally licensed cure for Nipah, but we are closer than ever.
- Supportive Care: The primary treatment remains intensive supportive care (hydration, ventilator support, seizure management).
- Monoclonal Antibodies (m102.4): This experimental therapy has been used on a “compassionate use” basis in India. In 2026, the Indian Council of Medical Research (ICMR) has intensified collaborations with Indian pharmaceutical companies to manufacture indigenous monoclonal antibodies to ensure readily available stock.
- Vaccines: Phase 2 clinical trials for the ChAdOx1 NipahB vaccine (developed by Oxford and the Serum Institute of India) are progressing. While not yet available for the general public, this offers hope for the near future.
Stay updated with the latest guidelines from the <a href=”https://ncdc.mohfw.gov.in/” target=”_blank”>National Centre for Disease Control (NCDC)</a>.
Prevention: Your Best Defense
Since treatment options are limited, prevention is absolute.
- Avoid Raw Date Palm Sap: In India and Bangladesh, this is the #1 cause of “spillover” events. Do not drink raw Toddy. If it must be consumed, it should be boiled first.
- Wash Fruits Thoroughly: Fruit bats love mangoes, guavas, and litchis. Discard any fruit that shows signs of bat bites or scratches. Wash and peel fruits before eating.
- Hand Hygiene: Wash hands frequently with soap and water, especially after visiting hospitals or caring for sick relatives.
- Use Masks: In outbreak zones (like the current alert areas in West Bengal), wear N95 masks in crowded places or near healthcare facilities.
- Isolate Patients: If a family member shows symptoms, isolate them immediately and call local health authorities. Do not attempt to nurse them without full protective gear.
A Personal Note to My Readers
I know reading about Nipah can be scary, especially with the news channels flashing alerts about the 2026 cases. But remember, Nipah is not airborne like COVID-19 in the general sense; it requires close contact or consumption of contaminated items.
My advice: Be vigilant, not paranoid. Stop drinking raw date palm sap immediately—it is simply not worth the risk. If you see a bat bitten fruit on the ground, do not touch it. And most importantly, if you or someone you know has a high fever with confusion or breathing trouble, do not self-medicate. Go to a hospital immediately and mention your travel history.
Call to Action: Knowledge saves lives. Share this article with your family and friends via WhatsApp and social media. The more people know about the symptoms of Nipah virus infection, the safer our community will be.
Disclaimer: This content is provided for general information only and is not a substitute for professional medical advice. Always seek guidance from a qualified healthcare provider for proper diagnosis and treatment.
Reference: <a href=”https://www.google.com/search?q=https://www.cdc.gov/nipah-virus/index.html” target=”_blank”>Centers for Disease Control and Prevention (CDC)</a>